Takeaway Message
Type A Aortic Dissection
1. Surgical emergency
2. Outcomes have improved over the last 20 years
3. Long-term aortic surveillance is mandatory
1. Surgical emergency
2. Outcomes have improved over the last 20 years
3. Long-term aortic surveillance is mandatory
Type A Aortic Dissection
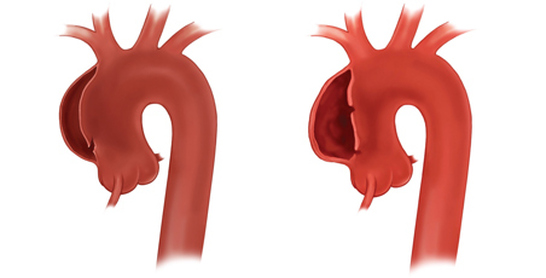
The illustration shows the tear in the inner lining and false channel of the ascending aorta.
An aortic dissection occurs when the inner layer (intima) of the aorta tears and blood passes through this separation through the aortic wall. The separation of the layers of the aortic wall produces a false channel (lumen), which spirals throughout a portion or commonly, the entire length of the aorta. In the United States, the prevalence of aortic dissection ranges from 0.2 to 0.8 per 100,000 per year or roughly 2,000 to 3,000 new cases per year.
An acute aortic dissection usually causes a severe sharp, tearing pain in the chest and upper back. In certain patients, the pain may develop or concentrate in the abdomen. In a very small number of patients, they may have little to no symptoms or flu-like symptoms.
The weakening of the aortic wall can lead to aortic rupture within minutes or hours of the acute event. The presence of the false channel in the ascending aorta can result in regurgitation of the aortic valve and myocardial infarction (heart attack). If the disturbance of aortic valve is significant this can lead to sudden symptoms of heart failure secondary to severe aortic valve regurgitation.
A piece of clot can dislodge or the true channel can be compressed causing a stroke or lack of blood flow to the intestines. The first symptoms of an acute dissection can be parlaysis, speech impairment or severe abdominal pain.
Once the acute dissection occurs, the patient's risk of death increases 1% per hour until patient has aortic repair.
Most patients that develop a Type A aortic dissection have a history of elevated blood pressure, an ascending aortic aneurysm, connective tissue disorder, bicuspid aortic valve, or have endured a stressful/emotional life event. The diagnosis is most commonly made based on history and symptoms however CT scan and/or echocardiogram are commonly used. A chronic Type A aortic dissection is rare because most patients are treated emergently with surgery.
An acute aortic dissection usually causes a severe sharp, tearing pain in the chest and upper back. In certain patients, the pain may develop or concentrate in the abdomen. In a very small number of patients, they may have little to no symptoms or flu-like symptoms.
The weakening of the aortic wall can lead to aortic rupture within minutes or hours of the acute event. The presence of the false channel in the ascending aorta can result in regurgitation of the aortic valve and myocardial infarction (heart attack). If the disturbance of aortic valve is significant this can lead to sudden symptoms of heart failure secondary to severe aortic valve regurgitation.
A piece of clot can dislodge or the true channel can be compressed causing a stroke or lack of blood flow to the intestines. The first symptoms of an acute dissection can be parlaysis, speech impairment or severe abdominal pain.
Once the acute dissection occurs, the patient's risk of death increases 1% per hour until patient has aortic repair.
Most patients that develop a Type A aortic dissection have a history of elevated blood pressure, an ascending aortic aneurysm, connective tissue disorder, bicuspid aortic valve, or have endured a stressful/emotional life event. The diagnosis is most commonly made based on history and symptoms however CT scan and/or echocardiogram are commonly used. A chronic Type A aortic dissection is rare because most patients are treated emergently with surgery.
Diagnosis

CTA scan of the chest
The diagnosis of a Type A aortic dissection is primarily based on clinical symptoms and radiographic imaging studies. The chest x-ray may provide the first suggestion of thoracic aortic pathology. The chest x-ray may show a pronounced heart shadow or silhouette indicating possible aortic aneurysm or aortic rupture. Obviously, the chest x-ray may tell the physician that another medical condition is causing the symptoms. An excellent study to diagnose an aortic dissection and is accessible in most emergency departments is a CT scan (or CT angiogram). MRI/A is also an excellent radiographic study, however, it is less accessible, more time consuming, and less patient-friendly. A transesophageal echocardiogram (TEE) is a very good study to diagnosis an aortic dissection, but it requires local and IV anesthesia and is also less accessible and patient-friendly.
A blood test that may increase the suspicion of an acute aortic dissection is D-dimer. However, D-dimer is elevated in other medical conditions. Some studies have suggested that if the D-dimer is above a certain level the likelihood of an aortic dissection is greater than 90% especially if the test is performed within 6 hours of onset of symptoms. As the time interval increases to 24 hours the sensitivity and specificity diminishes significantly. At this point, D-dimer can be used to stratify patients with symptoms suggestive of acute dissection to further imaging studies or continued observation.
A blood test that may increase the suspicion of an acute aortic dissection is D-dimer. However, D-dimer is elevated in other medical conditions. Some studies have suggested that if the D-dimer is above a certain level the likelihood of an aortic dissection is greater than 90% especially if the test is performed within 6 hours of onset of symptoms. As the time interval increases to 24 hours the sensitivity and specificity diminishes significantly. At this point, D-dimer can be used to stratify patients with symptoms suggestive of acute dissection to further imaging studies or continued observation.
Surgical Considerations
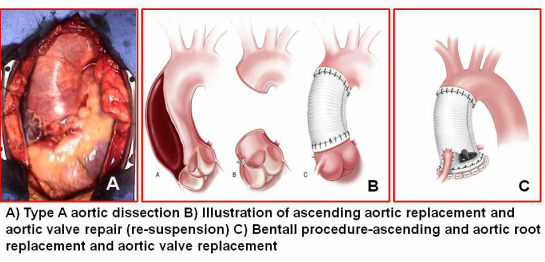
Emergency surgery is required to replace the ascending aorta with a prefabricated tubular prosthesis. The aortic valve may be repaired or replaced during the operation. Depending on the location of the intimal tear or involvement of the aortic arch vessel, more extensive surgery may be necessary. The main goal of the surgeon is to save the patient and if necessary, delay additional repair when patient has recovered from the acute dissection operation.
After any successful aortic repair, the patient will need life-long surveillance of their entire aorta especially the first two years. To sign-up for our aortic surveillance program.
After any successful aortic repair, the patient will need life-long surveillance of their entire aorta especially the first two years. To sign-up for our aortic surveillance program.
|
Delayed repair of acute type A aortic dissection in a patient with gastrointestinal bleeding and pulse deficit. Ann Thorac Surg. 2007 Dec;84(6):2097-9.
(click on image) |